FLCCC Alliance Prevention & Treatment Protocol for COVID-19
Below are the treatment protocols for COVID-19 as advocated by the Front Line COVID-19 Critical Care Alliance. Always consult with a medical professional before taking any medications and use this information at your own discretion.
I-MASK+ Prevention & Early Outpatient Treatment Protocol for COVID-19:
Click here to view the pdf
In October 2020, the FLCCC Alliance developed a preventive and early outpatient combination treatment protocol for COVID-19 called I-MASK+. It’s centered around ivermectin, a well-known, FDA-approved anti-parasite drug that has been used successfully for more than four decades to treat onchocerciasis “river blindness” and other parasitic diseases. It is one of the safest drugs known. It is on the WHO’s list of essential medicines, has been given 3.7 billion times around the globe, and has won the Nobel prize for its global and historic impacts in eradicating endemic parasitic infections in many parts of the world. Our medical discovery of a rapidly growing published medical evidence base, demonstrating ivermectin’s unique and highly potent ability to inhibit SARS-CoV-2 replication and to suppress inflammation, prompted our team to use ivermectin for prevention and treatment in all stages of COVID-19. Ivermectin is not yet FDA-approved for the treatment of COVID-19, but on Jan 14, 2021, the NIH changed their recommendation for the use of ivermectin in COVID-19 from “against” to “neutral”.
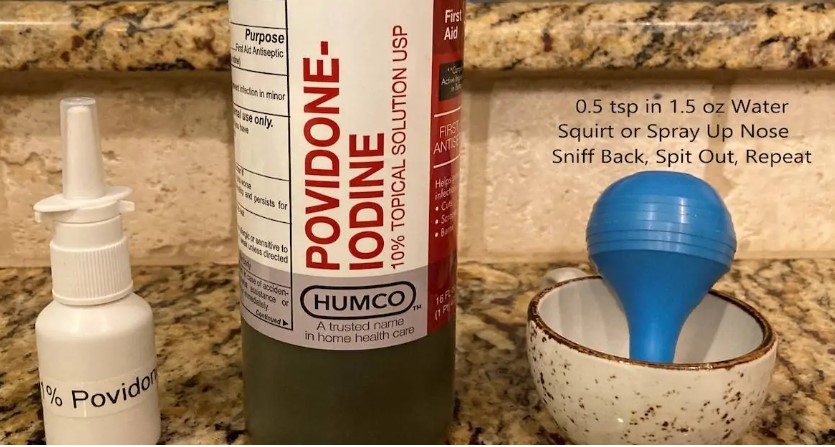
Dr McCullough’s Nasal/Throat Spray:
Click here to view
The MATH+ Hospital Treatment Protocol for COVID-19 is designed for hospitalized patients, to be initiated as soon as possible after they develop respiratory difficulty and require oxygen supplementation. The three core pathophysiologic processes that have been identified are severe hypoxemia, hyperinflammation, and hypercoagulability. This combination medication protocol is designed to counteract these processes either through the use of single agents or in synergistic actions. A unique insight into this disease made by members of our group is that the majority of patients initially present with an inflammatory reaction in the lungs called “organizing pneumonia,” which is the body’s reaction to injury and is profoundly responsive to corticosteroid therapy. If the organizing pneumonia response is left untreated or presents as a rapidly progressive sub-type, a condition called Acute Respiratory Distress Syndrome (ARDS) follows.
The two main therapies that can reverse and/or mitigate the extreme inflammation causing ARDS are the combination of the corticosteroid Methylprednisolone and the antioxidant Ascorbic acid, which is given intravenously and in high doses. Both of these medicines have multiple synergistic physiologic effects and have been shown in multiple randomized controlled trials to improve survival in ARDS, particularly when given early in the disease. Thiamine is given to optimize cellular oxygen utilization and energy consumption, protecting the heart, brain, and immune system. Given the numerous clinical and scientific investigations that have demonstrated consistent, reproducible, and excessive levels of hyper-coagulation, particularly in the severely ill, the anticoagulant Heparin is used to both prevent and help in dissolving blood clots that appear with a very high frequency. The “+” sign indicates several important co-interventions that have a combination of strong physiologic rationale with existing or emerging pre-clinical and clinical data to support their use in similar conditions or in COVID-19 itself, and all with a well-established safety profile. Such adjunctive therapies are continuously being evaluated and amended as the published medical evidence evolves.
Timing is a critical factor in the efficacy of MATH+ and to achieving successful outcomes in patients ill with COVID-19. Patients must go to the hospital as soon as they experience difficulty breathing or have a low oxygen level. The MATH+ protocol should be administered soon after a patient meets criteria for oxygen supplementation (within the first hours after arrival in the hospital), in order to achieve maximal efficacy. Delayed therapy can lead to complications such as the need for mechanical ventilation. If administered early, the MATH+ formula of FDA-approved, safe, inexpensive, and readily available drugs may eliminate the need for ICU beds and mechanical ventilators and return patients to health.
The Long Haul COVID-19 Syndrome (LHCS) is an often debilitating syndrome characterized by a multitude of symptoms such as prolonged malaise, headaches, generalized fatigue, sleep difficulties, smell disorder, decreased appetite, painful joints, dyspnea, chest pain and cognitive dysfunction. The incidence of symptoms after COVID-19 varies from as low as 10% to as high as 80%. LHCS is not only seen after the COVID-19 infection but it is being observed in some people that have received vaccines (likely due to monocyte activation by the spike protein from the vaccine). A puzzling feature of the LHCS syndrome is that it is not predicted by initial disease severity; post-COVID-19 frequently affects mild-to-moderate cases and younger adults that did not require respiratory support or intensive care.
The symptom set of LHCS in the majority of cases is very similar to the chronic inflammatory response syndrome (CIRS)/myalgic encephalomyelitis/chronic fatigue syndrome, although in LHCS, symptoms tend to improve slowly in the majority of the cases. Furthermore, the similarity between the mast cell activation syndrome and LHCS has been observed, and many consider post-COVID-19 to be a variant of the mast cell activation syndrome. LHCS is highly heterogenous and likely results from a variety of pathogenetic mechanisms. Furthermore, it is likely that delayed treatment (with ivermectin) in the early symptomatic phase will result in a high viral load, which increases the risk and severity of LHCS.
Although numerous reports describe the epidemiology and clinical features of LHCS, studies evaluating treatment options are glaringly sparse. Indeed, the NICE guideline for managing the long-term effects of COVID-19 provide no specific pharmacologic treatment recommendations.
Given the lack of available treatment recommendations in the setting of large numbers of patients suffering with this disorder globally, the FLCCC developed the I-RECOVER protocol in collaboration with a number of expert clinicians including Dr. Mobeen Syed, Dr. Ram Yogendra, Dr. Bruce Patterson, and Dr. Tina Peers. Although our varied yet often overlapping treatment approaches were initially empiric, while based on both preliminary investigations into and prevailing theoretical pathophysiologic mechanisms of LHCS, the consistently positive clinical responses observed, often profound and sustained, led the collaboration to form the consensus protocol below. As with all FLCCC protocols, we must emphasize that multiple aspects of the protocol may change as scientific data and clinical experience in this condition evolve, thus it is important to check back frequently or join the FLCCC Alliance to receive notification of any protocol changes.